New program at St. James aims to help improve stoke awareness by encouraging people to B.E. F.A.S.T.
May is Stroke Awareness Month

After a stroke, every minute counts. Every minute you wait could be the difference between being able to communicate, being able to walk, being able to brush your hair, or holding your grandkids.
The typical person loses 1.9 million neurons each minute that a stroke is untreated.
In Butte, new data shows most individuals who experience a stroke are not getting treatment in time.
“A lot of our patients show up more than a day outside of an event,” said Amanda Opfer, DO. She specializes in emergency medicine and is one of the providers at St. James Healthcare who will be the first to treat an individual presenting with stroke.
The risk factors of stroke include, but are not limited to: smoking, high blood pressure, heart disease, diabetes, high cholesterol, obesity, and lack of exercise. For the prevention of stroke, it is important to have regular follow-up appointments with your primary care provider.
New numbers collected as part of the stroke care program show that 20 people suffering strokes came into the Butte emergency room so far this year and 14 of those were outside of the window to receive the actual intervention.
If you look in the mirror and one side of your face is drooping, or you notice any asymmetry — that could be a sign you’re having a stroke. You might take a sip of water or coffee and you drool or drip on your clothes.
If you’re talking with a loved one all of a sudden their speech is kind of garbled or slurred sounding, they should get checked.
Other common symptoms are issues moving one side of your body, feeling off-balance, or blurred vision. If you experience any of these or see someone who is experiencing them, then you need to think about time and get to an emergency room as soon as possible.
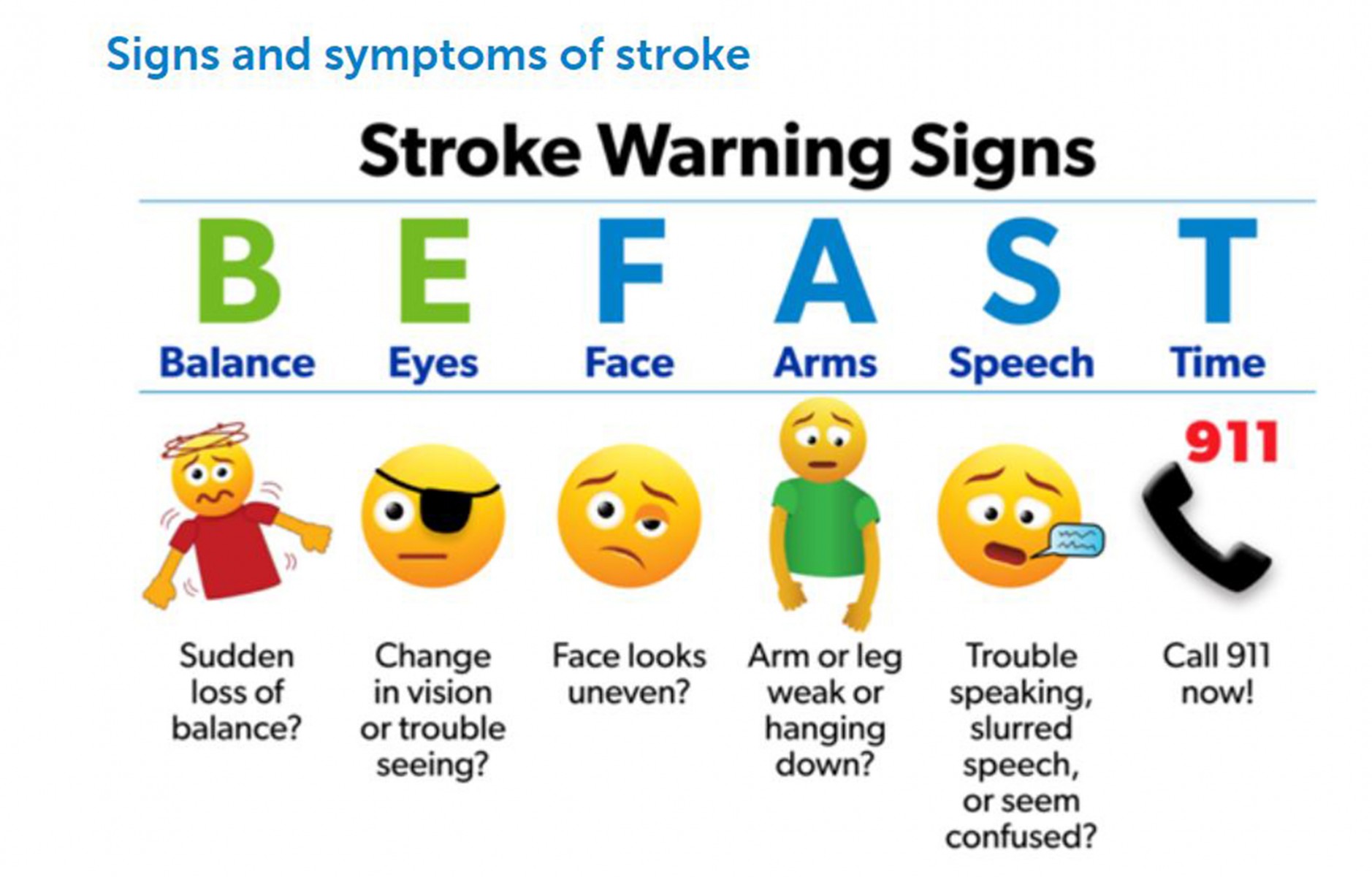
An acronym to remember is B.E. F.A.S.T. (Balance, eyes, face, arms, speech, and time). People experiencing symptoms should call 911 immediately. Do not attempt to drive yourself, it is best to call for an ambulance as they can ensure you arrive at the hospital safely and they can inform the Emergency Department of your arrival.
“What we see is people will start to experience symptoms and they won’t come in for 24 hours; then it’s too late for one type of intervention,” said Kelly Brock, PT, DPT, a physical therapist, and the stroke program coordinator at St. James Healthcare.
The intervention Brock and Opfer are referring to is tPA, tissue plasminogen activator, also known as a clot buster. It’s a type of heart medication given through an IV to break up blood clots but it can only be used within a four-hour window after a stroke has occurred.
Only two of the twenty stroke patients in Butte received the tPA.
A stroke is a lack of oxygen, a lack of blood flow to a part of the brain. There are two kinds of stroke — ischemic and hemorrhagic stroke. Ischemic happens when there is a blockage in a blood vessel and accounts for 85% of strokes. Hemorrhagic strokes are rarer and happen with a vessel that feeds your brain ruptures and there is bleeding.
The long-term effects of a stroke can vary wildly. Opfer says it depends on where the clot or bleeding is and what part of the brain is affected.

People always ask what they can do to prevent a stroke in the future and what I tell them is to make sure you are following closely with their primary care provider and get their cholesterol checked, make sure their blood pressure is controlled, and to avoid smoking. Doing these small interventions can make a big difference in reducing your risk of stroke.
“The brain is super-specialized and it is fed by a bunch of different pathways,” she explained. “There are some people who can get their function back if they come into the ER soon enough — in that three to four-hour window.”
But she said it’s still good to be treated, even if you didn’t make it to the hospital right away.
“If somebody isn’t a candidate for that tPA medication or their symptoms have been going on for too long and we can’t give it to them, it doesn’t mean that there is nothing that can be done — we have a great therapy department at the hospital that helps work with people who have had a stroke to help them get some of their abilities back.”
A little over a year ago, the hospital received a $72,000 grant from American Heart Association’s Montana Mission: Lifeline® Stroke. Mission: Lifeline Stroke aims to transform stroke care by focusing efforts on connecting all of the components of acute stroke care into a smoothly integrated system that reinforces the use of evidence-based guidelines, measures performance, identifies gaps, and engages in improvement projects at a systems level.
“This is a brand new program that the hospital is building. We’ve always had stroke care but the goal is to get Joint Commission certified, to have that gold standard of care,” said Brock.
She’s heading the program aimed at achieving Acute Stroke Ready Hospital (ASRH) Certification through the Joint Commission with the support of the American Heart Association. The first part of the program has been data collection and working to get the necessary pieces in place. Next, they’ll work on additional staff and community education. Feedback forms are going to providers and nurses that see patients in the emergency room and the EMS crew.
Brock is passionate about the stroke care program. Eventually, there will be one person from every department on the stroke committee and she is looking forward to interacting with all the individuals who provide care for a patient during their time in the hospital

We’re able to have discussions that really involve the full continuum of care for somebody from the moment they come into the hospital to the moment they’re discharged or go to outpatient therapy.
The Stroke team will be participating in health fairs, and eventually will have additional community education opportunities planned, to help get the word out about symptoms that require immediate attention.
“I think the main thing I would like people to know is to remember not to wait. If they’re having those symptoms — don’t wait and see if it will just go away,” said Opfer. “That is, unfortunately, something I hear a lot. Maybe they have difficulty talking and they have difficulty for maybe 20 minutes, and then everything goes back to normal. A lot of people will stay home if that happens.”
She said that doesn’t mean a patient is in the clear. It could be a mini-stroke and a warning sign that they have something larger impending.
Stroke is a leading cause of adult disability. The most common types of disability after stroke are impaired speech, restricted physical abilities, weakness or paralysis of limbs, difficulty gripping or holding things, and a slowed ability to communicate.
“People always ask what they can do to prevent a stroke in the future and what I tell them is to make sure you are following closely with your primary care provider and get your cholesterol checked, making sure your blood pressure is controlled, and to avoid smoking,” said Opfer. “Doing these small interventions can make a big difference in reducing your risk of stroke.”
Written by McKayla Haack
McKayla is a Montana native who’s called Butte home for three years. She’s been sharing stories from Big Sky Country for nearly a decade and is honored to share the stories of St. James Healthcare patients and providers.
In the media
Stroke Awareness: New program aims to improve statistics by encouraging people to B.E. F.A.S.T.
About St. James Healthcare and Intermountain Healthcare
St. James Healthcare has served the people of Southwestern Montana for more than 135 years and is the largest and only acute care health care facility in the region. St. James Healthcare is a 67-bed hospital located in Butte, Montana, with more than 450 caregivers, alongside 100 physicians and advanced care professionals, offering 24-hour care and dozens of progressive specialty services. St. James Healthcare is part of the Intermountain Healthcare system. Based in Utah with locations in seven states (Montana, Colorado, Idaho, Kansas, Nevada, Utah, and Wyoming) and additional operations across the western U.S., Intermountain Healthcare is a nonprofit healthcare system comprised of 33 hospitals, 385 clinics, medical groups with some 3,800 employed physicians and advanced practice providers. To help people live the healthiest lives possible, Intermountain is committed to improving community health and is widely recognized as a leader in transforming healthcare by using evidence-based best practices to consistently deliver high-quality outcomes at sustainable costs. To learn more about St. James Healthcare, visit sjh-mt.org.



